Special Senses
Vision
By the end of this module you will be able to:
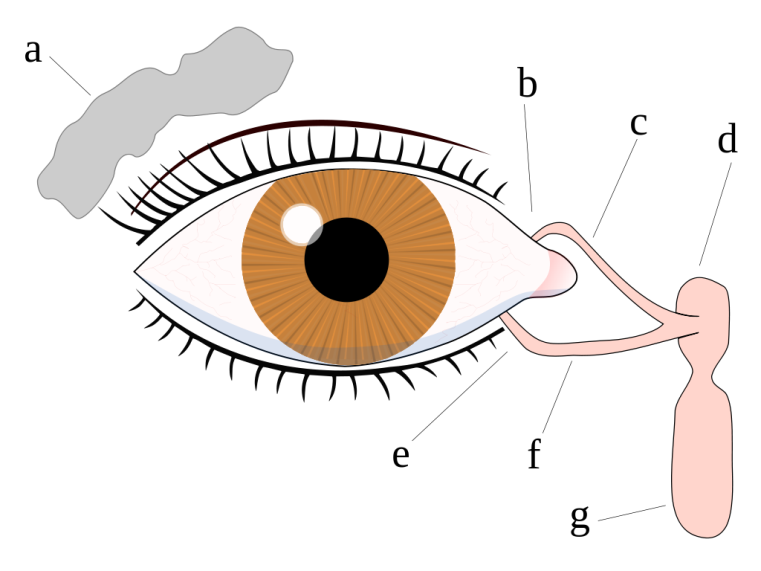
Vision is a special sense that involves the transduction (conversion) of wavelengths or particles of light called photons into nerve impulses at the eye, sending these impulses to the brain and then interpreting these impulse into images by the visual cortex of the brain. The eyes are located in the orbital sockets of the skull and surrounded by a series of accessory structures that include the eyelids, eyelashes, muscles, lacrimal (tear) glands, and mucous membranes. The eyelids, with the eyelashes, help to protect the eye from damage by blocking material from entering the eye. The inner part of the eyelid as well as the outer part of the eye is lined with a membrane called the conjunctiva. The part of the conjunctiva that lines the eyelid is called the palpebral conjunctiva. This then connects the eyelids to the eyeball. On the lateral edge of the eye is the lacrimal gland that produces tears. Tears flow through the lacrimal duct to the inner corner of the eye washing foreign particles from the eye, where they drain into a duct that connects to the nasal cavity. In addition to cleansing the eye, these tears also contain an enzyme called lysozyme that helps to protect the eye against infections.
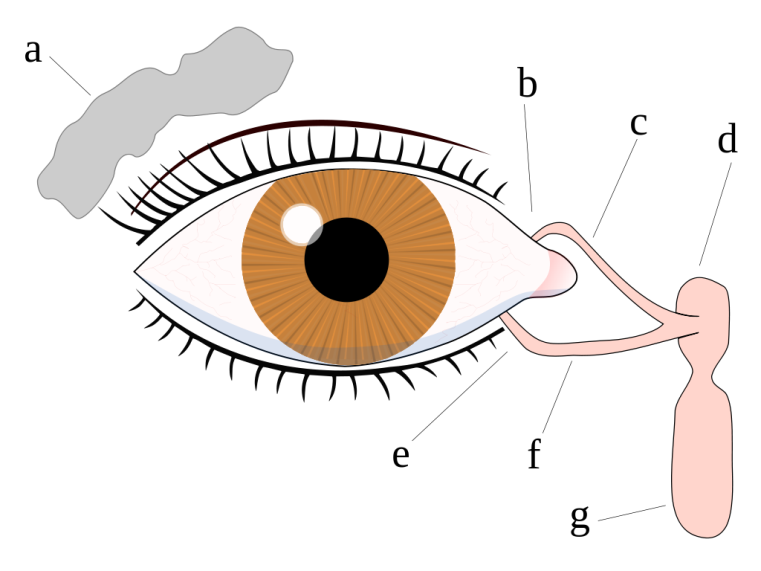
Figure 1: The Lacrimal apparatus and the drainage of tears start with the lacrimal gland in the upper side of the eye to the lower corner of the eye through which tears drains into the nasal cavity. The lacrimal gland in the upper side of the eye is colored gray while the lacrimal apparatus consisting of the canals and the nasolacrimal duct are colored pink. a. tear gland / lacrimal gland, b. superior lacrimal punctum/opening, c. superior lacrimal canal, d. tear sac / lacrimal sac, e. inferior lacrimal punctum, f. inferior lacrimal canal, g. nasolacrimal canal
The eye is moved by six extraocular muscles, also known as extrinsic eye muscles. These muscles originate from the bones of the orbit and insert into the surface of the eyeball. There are six muscles that are present in the orbit (eye socket) that attach to the eye to move it. These muscles work to move the eye up and down, side to side, and to rotate the eye. The superior rectus is an extraocular muscle that attaches to the anterior, superior surface eye. It moves the eye upward. The inferior rectus is an extraocular muscle that attaches to the anterior, inferior surface eye. It moves the eye downward. The medial rectus is an extraocular muscle that attaches to the anterior, medial surface eye near the nose. It moves the eye inward toward the nose. The lateral rectus is an extraocular muscle that to the attaches anterior, lateral surface of the eye near the temple. It moves the eye outward.
The superior oblique is an extraocular muscle that comes from the back of the orbit and attaches to the posterior, superior, lateral surface eye. This muscle threads through a pulley-like piece of cartilage known as the trochlea. The superior oblique rotates the eye inward around the long axis of the eye (front to back). The superior oblique also moves the eye downward.
The inferior oblique is an extraocular muscle that attaches to the posterior, inferior, lateral surface of the orbit near the nose. It then travels outward and backward in the orbit before attaching to the bottom part of the eyeball. It rotates the eye outward along the long axis of the eye (front to back). The inferior oblique also moves the eye upward.
A seventh muscle in the orbit is the levator palpebrae superioris, which is responsible for elevating and retracting the upper eyelid, a movement that usually occurs in concert with elevation of the eye by the superior rectus.
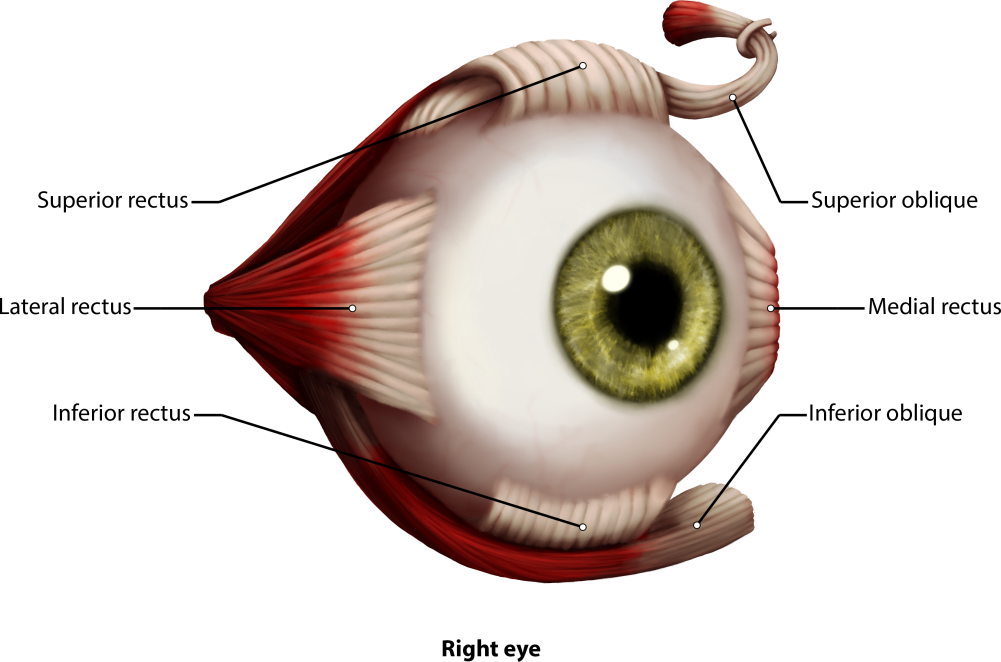
Figure 2: The eye and the six different extrinsic eye muscles. All muscles are colored reddish brown in the picture with white tendinous attachments to the eye. The superior rectus, lateral rectus, inferior rectus, inferior oblique, medial rectus and the superior oblique muscle as well as the trochlea are shown.
The muscles of the eye are innervated by three cranial nerves. Most of the muscles of the eye are innervated by the oculomotor nerve (cranial nerve III). The lateral rectus is innervated by the abducens nerve, CN IV, which causes abduction of the eye. The trochlear nerve, CN VI, innervates the superior oblique.
Strabismus (related to lazy eye) - Strabismus is a failure of the two eyes to maintain proper alignment and work together as a team. Some babies' eyes may appear to be misaligned, but are actually both aiming at the same object.
Strabismus is classified by the direction the eye turns:
In ophthalmology the Cardinal Gaze tests one of six positions to which the normal eye may be turned. This test evaluates the functioning of the six extraocular muscles and the three corresponding cranial nerves. The positions and the corresponding muscles and nerves are:
The eye is composed of three main layers or coats of tissues called tunics. The outermost layer is the fibrous tunic, which includes the white sclera and clear cornea. The sclera accounts for five sixths of the surface of the eye, most of which is not visible, though humans are unique compared with many other species in having so much of the "white of the eye" visible (Figure 3). The transparent cornea covers the anterior tip of the eye and allows light to enter the eye. This cornea is one of two major structures, along with the lens, in the eye that will cause light to bend and be focused on the posterior or back of the eye, where special types of receptors called photoreceptors are located. The middle layer of the eye is the vascular tunic, which is mostly composed of the choroid, ciliary body, and iris. The choroid is a layer of highly vascularized connective tissue that provides a blood supply to the eyeball. The choroid is posterior to the ciliary body, a muscular structure that is attached to the lens by zonule fibers (also called suspensory ligaments). These two structures bend the lens, allowing it to focus light on the back of the eye. Overlaying the ciliary body, and visible in the anterior eye, is the iris—the colored part of the eye. The iris is a smooth muscle that opens or closes the pupil, which is the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light. The innermost layer of the eye is the neural tunic, or retina, which contains the nervous tissue responsible for photoreception.
The eye is also divided into two cavities: the anterior cavity and the posterior cavity. The anterior cavity is the space between the cornea and lens, including the iris and ciliary body. It is filled with a watery fluid called the aqueous humor. The anterior cavity is also divided up into two chambers: the anterior chamber and the posterior chamber. The posterior chamber contains the lens and the ciliary bodies. It is at the ciliary bodies that the secretion of the aqueous humor take places derived from capillaries in their walls. The aqueous humor then circulates into the anterior chamber through the pupil and is then returned to the blood through the scleral venous sinus, that is a small opening found at the junction of the cornea and sclera. This opening allows for the drainage of aqueous humor from the anterior compartment of the eye and, therefore, reducing intraocular pressure related to glaucoma.The posterior cavity is the space behind the lens that extends to the posterior side of the interior eyeball, where the retina is located. The posterior cavity (vitreous chamber) is filled with a more viscous fluid called the vitreous humor.
The retina is composed of several layers and contains specialized cells for the initial processing of visual stimuli. The photoreceptors (rods and cones) change their membrane potential when stimulated by light energy. The change in membrane potential alters the amount of neurotransmitter that the photoreceptor cells release onto bipolar cells in the outer synaptic layer. It is the bipolar cell in the retina that connects a photoreceptor to a retinal ganglion cell (RGC) in the inner synaptic layer. There, amacrine cells additionally contribute to retinal processing before an action potential is produced by the RGC. The axons of RGCs, which lie at the innermost layer of the retina, collect at theoptic disc and leave the eye as the optic nerve (see Figure 3). Because these axons pass through the retina, there are no photoreceptors at the very back of the eye, where the optic nerve begins. This creates a "blind spot" in the retina, and a corresponding blind spot in our visual field.
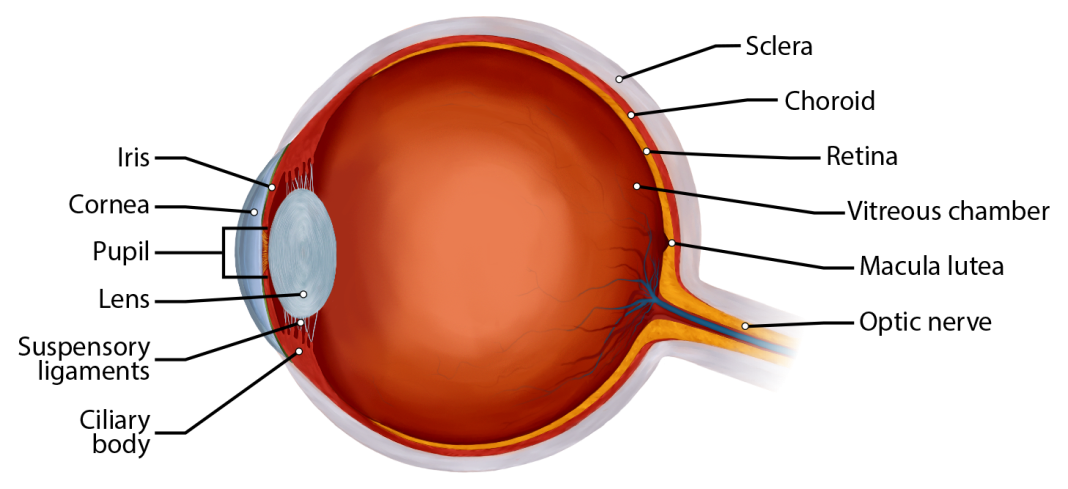
Figure 3: This picture shows a section through an eye showing most of the major parts of the eye such as the sclera, cornea, choroid, retina, the macula lutea (with the fovea in the center), optic nerve, suspensory ligaments, lens, iris, pupil, ciliary bodies, and the two major cavities of the eye (anterior cavity, anterior to the lens, and vitreous chamber or posterior cavity).
Now we will examine the microscopic level of the retina.
Understand that the photoreceptors in the retina (rods and cones) are located behind the axons, RGCs, bipolar cells, and retinal blood vessels. A significant amount of light is absorbed by these structures before the light reaches the photoreceptor cells. However, at the exact center of the retina is a small area known as the macula, which has the central fovea. At the fovea, the retina lacks the supporting cells and blood vessels, and only contains photoreceptors. Therefore, visual acuity, or the sharpness of vision, is greatest at the fovea. This is because the fovea is where the least amount of incoming light is absorbed by other retinal structures (see Figure 4). As one moves in either direction from this central point of the retina, visual acuity drops significantly. In addition, each photoreceptor cell of the fovea is connected to a single RGC. Therefore, this RGC does not have to integrate inputs from multiple photoreceptors, which reduces the accuracy of visual transduction. Toward the edges of the retina, several photoreceptors converge on RGCs (through the bipolar cells) up to a ratio of 50 to 1. The difference in visual acuity between the fovea and peripheral retina is easily evidenced by looking directly at a word in the middle of this paragraph. The visual stimulus in the middle of the field of view falls on the fovea and is in the sharpest focus. Without moving your eyes off that word, notice that words at the beginning or end of the paragraph are not in focus. The images in your peripheral vision are focused by the peripheral retina, and have vague, blurry edges and words that are not as clearly identified. As a result, a large part of the neural function of the eyes is concerned with moving the eyes and head so that important visual stimuli are centered on the fovea.
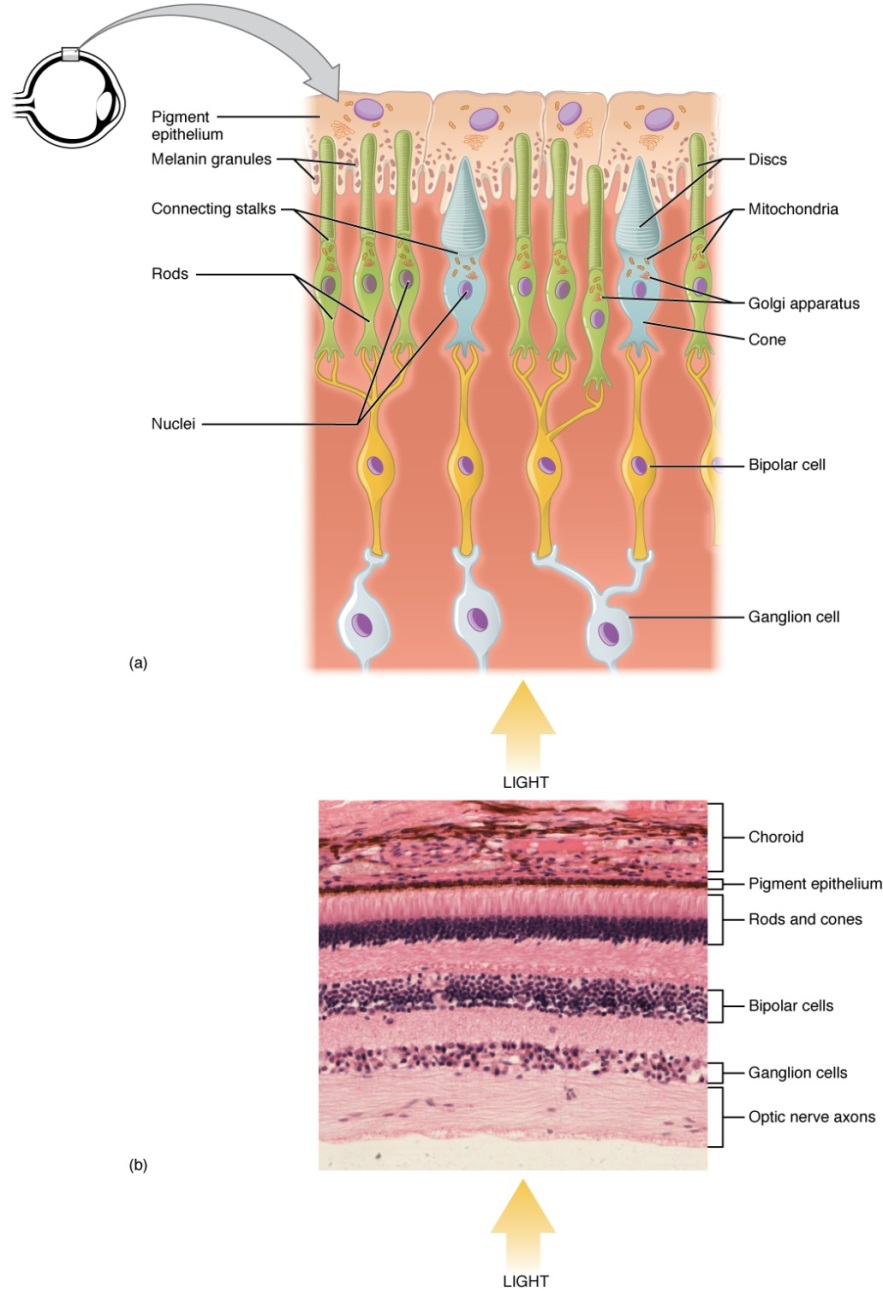
Figure 4. The Retina showing the direction that light passes on the retina. Notice that light passes through several layers of cells before reaching the rods and cones in the back of the eye. The cells that light passes through include ganglion cells, bipolar cells, rods and cones before it reaches the pigment epithelium. Notice also that the disc of the photoreceptors determines its name. The rods for example have rod shaped discs, while the cones have a disc that looks like an upside down cone.
Light falling on the retina causes chemical changes to pigment molecules in the photoreceptors, ultimately leading to a change in the activity of the RGCs. Photoreceptor cells have two parts, the inner segment and the outer segment (Figure 4). The inner segment contains the nucleus and other common organelles of a cell, whereas the outer segment is a specialized region in which photoreception takes place. There are two types of photoreceptors—rods and cones—which differ in the shape of their outer segment. The rod-shaped outer segments of the rod photoreceptor contain a stack of membrane-bound discs that contain the photosensitive pigment rhodopsin. The cone-shaped outer segments of the cone photoreceptor contain their photosensitive pigments in infoldings of the cell membrane. There are three cone photopigments, called opsins, which are each sensitive to a particular wavelength of light. The wavelength of visible light determines its color. The pigments in human eyes are specialized in perceiving three different primary colors: red, green, and blue.
At the molecular level, visual stimuli cause changes in the photopigment molecule that lead to changes in membrane potential of the photoreceptor cell. A single unit of light is called a photon, which is described in physics as a packet of energy with properties of both a particle and a wave. The energy of a photon is represented by its wavelength, with each wavelength of visible light corresponding to a particular color. Visible light is electromagnetic radiation with a wavelength between 380 and 720 nm. Wavelengths of electromagnetic radiation longer than 720 nm fall into the infrared range, whereas wavelengths shorter than 380 nm fall into the ultraviolet range. Light with a wavelength of 380 nm is blue whereas light with a wavelength of 720 nm is dark red. All other colors fall between red and blue at various points along the wavelength scale.
Opsin pigments are actually transmembrane proteins that contain a cofactor known as retinal. Retinal is a hydrocarbon molecule related to vitamin A. When a photon hits retinal, the long hydrocarbon chain of the molecule is biochemically altered. Specifically, photons cause some of the double-bonded carbons within the chain to switch from a cis to a trans conformation. This process is called photoisomerization. Before interacting with a photon, retinal's flexible double-bonded carbons are in the cis conformation. This molecule is referred to as 11-cis-retinal. A photon interacting with the molecule causes the flexible double-bonded carbons to change to the trans- conformation, forming all-trans-retinal, which has a straight hydrocarbon chain (Figure 5).
The shape change of retinal in the photoreceptors initiates visual transduction in the retina. Activation of retinal and the opsin proteins result in activation of a G protein. The G protein changes the membrane potential of the photoreceptor cell, which then releases less neurotransmitter into the outer synaptic layer of the retina. Until the retinal molecule is changed back to the 11-cis-retinal shape, the opsin cannot respond to light energy, which is called bleaching. When a large group of photopigments is bleached, the retina will send information as if opposing visual information is being perceived. After a bright flash of light, afterimages are usually seen in negative. The photoisomerization is reversed by a series of enzymatic changes so that the retinal responds to more light energy.
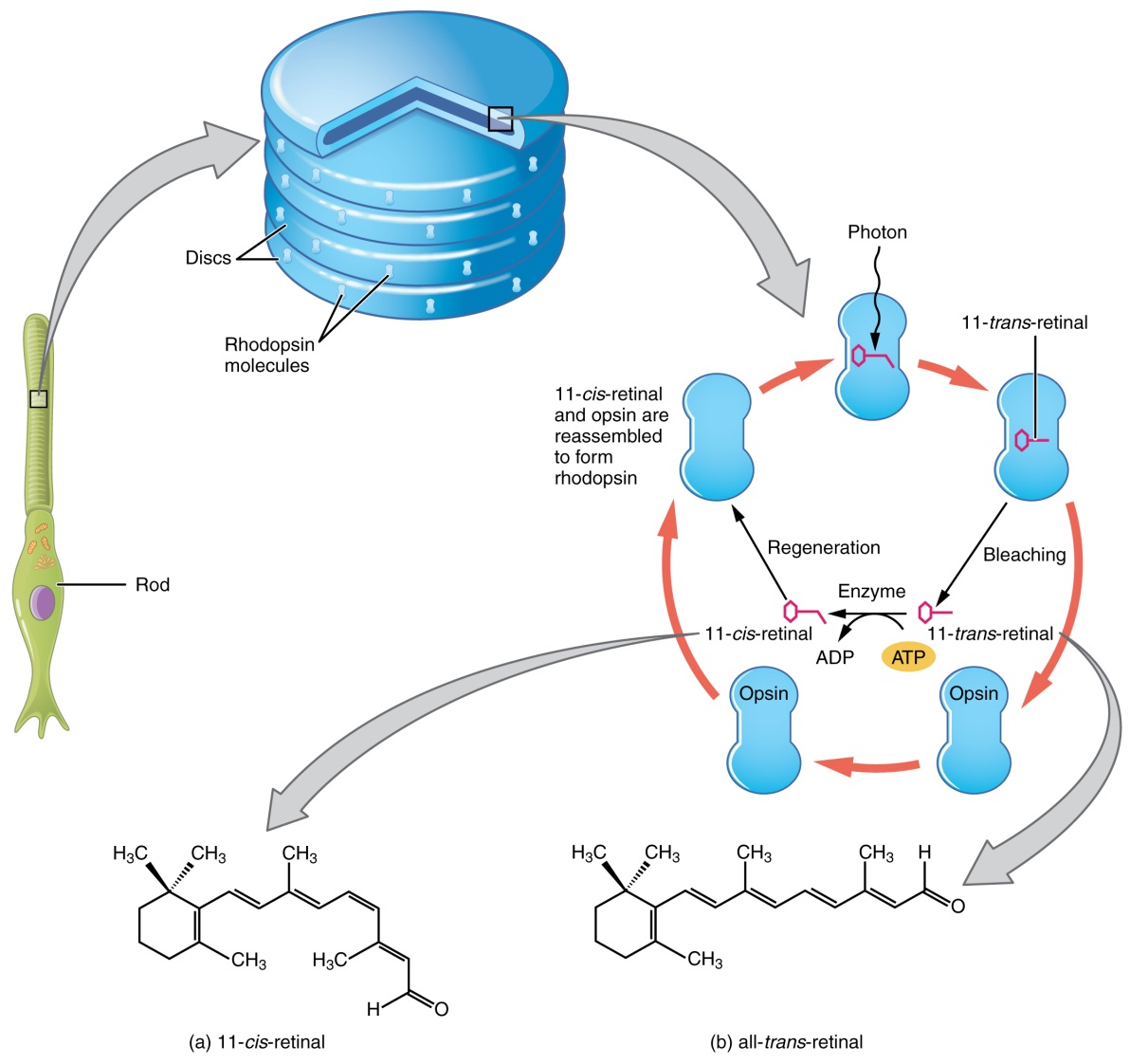
Figure 5: The retinal molecule has two isomers, (a) one before a photon interacts with it and (b) one that is altered through photoisomerization.
The opsins are sensitive to limited wavelengths of light. Rhodopsin, the photopigment in rods, is most sensitive to light at a wavelength of 498 nm. The three color opsins have peak sensitivities of 564 nm, 534 nm, and 420 nm corresponding roughly to the primary colors of red, green, and blue (Figure 6). The absorbance of rhodopsin in the rods is much more sensitive than in the cone opsins; specifically, rods are sensitive to vision in low light conditions, and cones are sensitive to brighter conditions. In normal sunlight, rhodopsin will be constantly bleached while the cones are active. In a darkened room, there is not enough light to activate cone opsins, and vision is entirely dependent on rods. Rods are so sensitive to light that a single photon can result in an action potential from a rod's corresponding RGC.
The three types of cone opsins, being sensitive to different wavelengths of light, provide us with color vision. By comparing the activity of the three different cones, the brain can extract color information from visual stimuli. For example, a bright blue light that has a wavelength of approximately 450 nm would activate the "red" cones minimally, the "green" cones marginally, and the "blue" cones predominantly. The relative activation of the three different cones is calculated by the brain, which perceives the color as blue. However, cones cannot react to low-intensity light, and rods do not sense the color of light. Therefore, our low-light vision is, in essence, in grayscale. In other words, in a dark room, everything appears as a shade of gray. If you think that you can see colors in the dark, it is most likely because your brain knows what color something is and is relying on that memory.
Comparison of Color Sensitivity of Photopigments
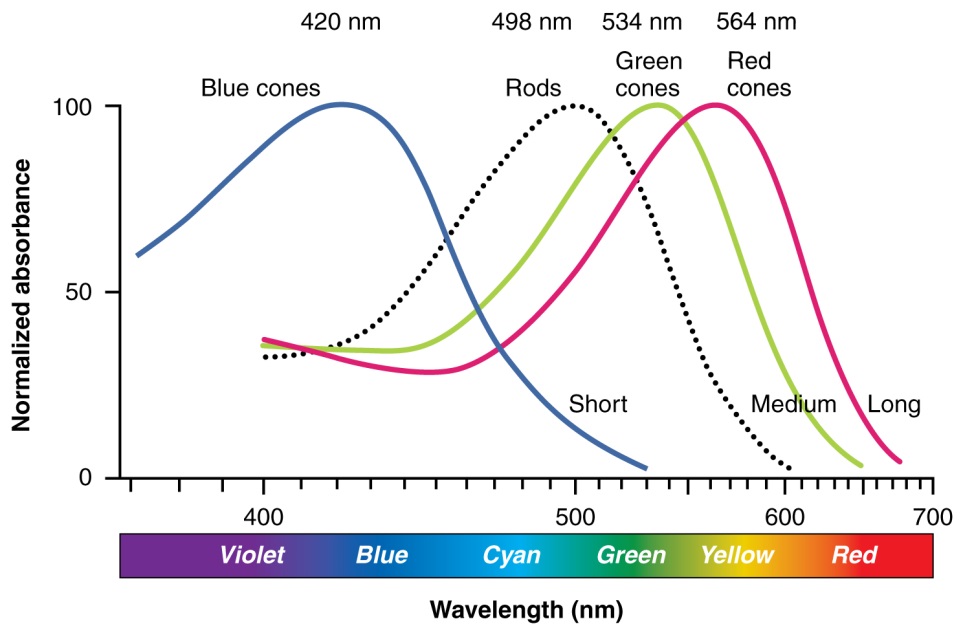
Figure 6: Comparing the peak sensitivity and absorbance spectra of the four photopigments suggests that they are most sensitive to particular wavelengths. Blue cones react to wavelengths of light close to 420nm. Green cones will react to wavelengths close to 530nm, and Red cones will react to those near 560nm.
Connections between the vestibular system and the cranial nerves controlling eye movement keep the eyes centered on a visual stimulus, even though the head is moving. During head movement, the eye muscles move the eyes in the opposite direction as the head movement, keeping the visual stimulus centered in the field of view.
The connections of the optic nerve are more complicated than those of other cranial nerves. Instead of the connections being between each eye and the brain, visual information is segregated between the left and right sides of the visual field. In addition, some of the information from one side of the visual field projects to the opposite side of the brain. Within each eye, the axons projecting from the medial side of the retina decussate at the optic chiasm. For example, the axons from the medial retina of the left eye cross over to the right side of the brain at the optic chiasm. However, within each eye, the axons projecting from the lateral side of the retina do not decussate. For example, the axons from the lateral retina of the right eye project back to the right side of the brain. Therefore the left field of view of each eye is processed on the right side of the brain, whereas the right field of view of each eye is processed on the left side of the brain (Figure 7).
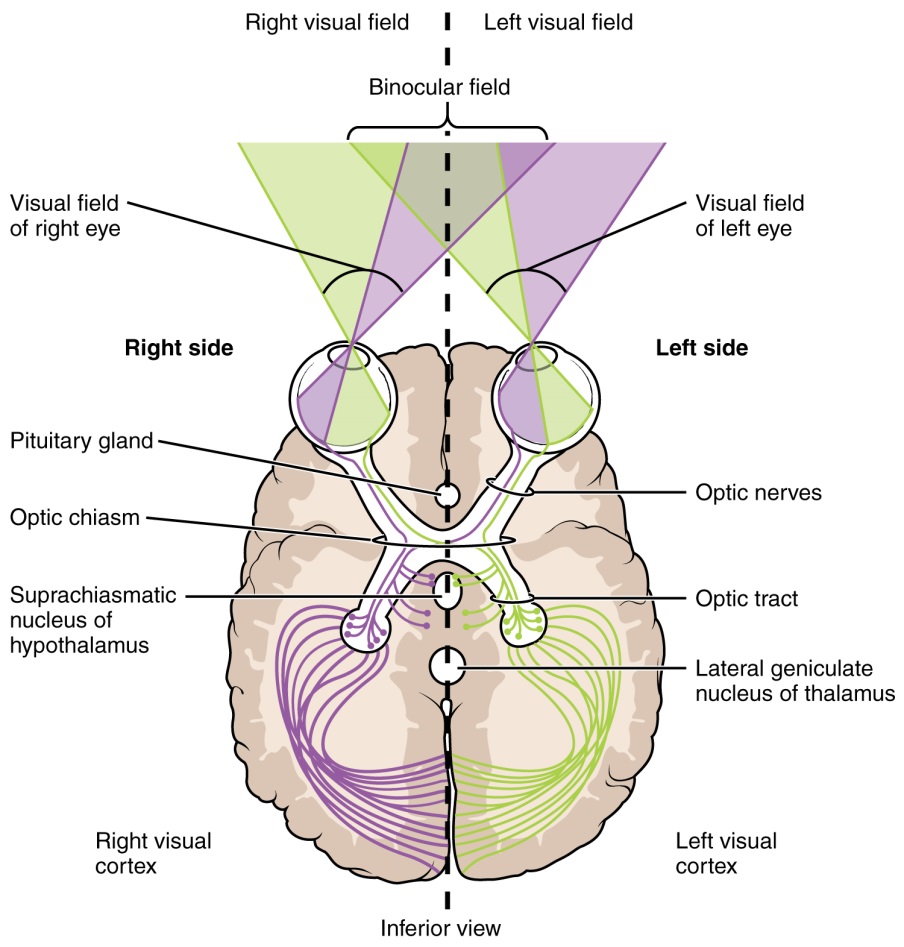
Figure 7: Contralateral visual field information from the lateral retina projects to the ipsilateral brain, whereas ipsilateral visual field information has to decussate (crossover) at the optic chiasm to reach the opposite side of the brain.
A unique clinical presentation that relates to this anatomic arrangement is the loss of lateral peripheral vision, known as bilateral hemianopia. This is different from "tunnel vision" because the superior and inferior peripheral fields are not lost. Visual field deficits can be disturbing for a patient, but in this case, the cause is not within the visual system itself. A growth of the pituitary gland presses against the optic chiasm and interferes with signal transmission. However, the axons projecting to the same side of the brain are unaffected. Therefore, the patient loses the outermost areas of their field of vision and cannot see objects to their right and left.
Extending from the optic chiasm, the axons of the visual system are referred to as the optic tract instead of the optic nerve. The optic tract has three major targets, two in the diencephalon and one in the midbrain. The connection between the eyes and diencephalon is demonstrated during development, in which the neural tissue of the retina differentiates from that of the diencephalon by the growth of the secondary vesicles. The connections of the retina into the CNS are a holdover from this developmental association. The majority of the connections of the optic tract are to the thalamus—specifically, the lateral geniculate nucleus. Axons from this nucleus then project to the visual cortex of the cerebrum, located in the occipital lobe. Another target of the optic tract is the superior colliculus.
In addition, a very small number of RGC axons project from the optic chiasm to the suprachiasmatic nucleus of the hypothalamus. These RGCs are photosensitive, in that they respond to the presence or absence of light. Unlike the photoreceptors, however, these photosensitive RGCs cannot be used to perceive images. By simply responding to the absence or presence of light, these RGCs can send information about day length. The perceived proportion of sunlight to darkness establishes the circadian rhythm of our bodies, allowing certain physiological events to occur at approximately the same time every day.
In the cerebral cortex, sensory processing begins at the primary sensory cortex, then proceeds to an association area, and finally, into a multimodal integration area. For example, the visual pathway projects from the retinae through the thalamus to the primary visual cortex in the occipital lobe. This area is primarily in the medial wall within the longitudinal fissure. Here, visual stimuli begin to be recognized as basic shapes. Edges of objects are recognized and built into more complex shapes. Also, inputs from both eyes are compared to extract depth information. Because of the overlapping field of view between the two eyes, the brain can begin to estimate the distance of stimuli based on binocular depth cues.
The centers of the two eyes are separated by a small distance, which is approximately 6 to 6.5 cm in most people. Because of this offset, visual stimuli do not fall on exactly the same spot on both retinae unless we are fixated directly on them and they fall on the fovea of each retina. All other objects in the visual field, either closer or farther away than the fixated object, will fall on different spots on the retina. When vision is fixed on an object in space, closer objects will fall on the lateral retina of each eye, and more distant objects will fall on the medial retina of either eye (Figure). This is easily observed by holding a finger up in front of your face as you look at a more distant object. You will see two images of your finger that represent the two disparate images that are falling on either retina.
These depth cues, both monocular and binocular, can be exploited to make the brain think there are three dimensions in two-dimensional information. This is the basis of 3-D movies. The projected image on the screen is two dimensional, but it has disparate information embedded in it. The 3-D glasses that are available at the theater filter the information so that only one eye sees one version of what is on the screen, and the other eye sees the other version. If you take the glasses off, the image on the screen will have varying amounts of blur because both eyes are seeing both layers of information, and the third dimension will not be evident. Some optical illusions can take advantage of depth cues as well, though those are more often using monocular cues to fool the brain into seeing different parts of the scene as being at different depths.
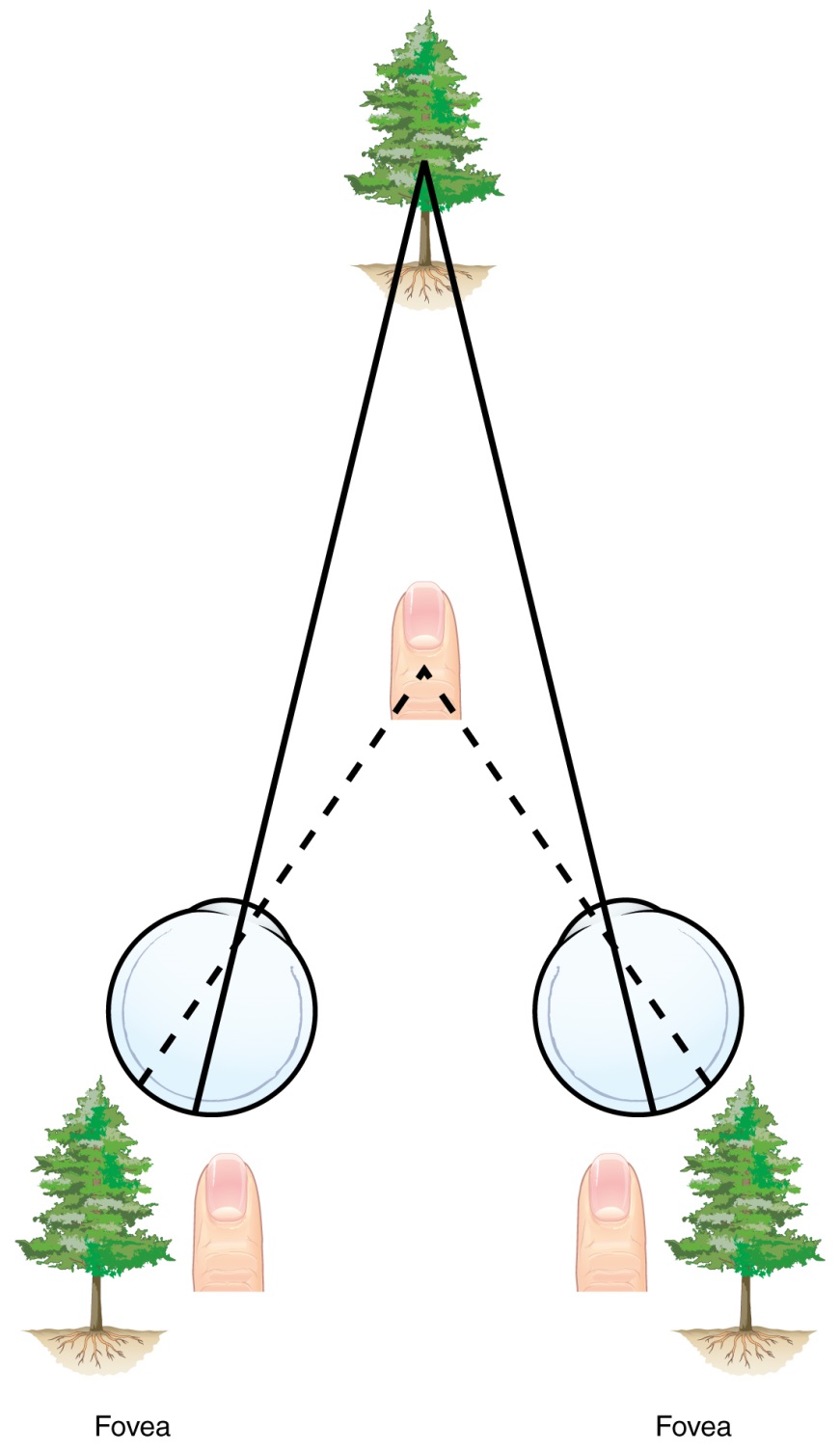
Figure 8: Because of the interocular distance, which results in objects of different distances falling on different spots of the two retinae, the brain can extract depth perception from the two-dimensional information of the visual field. If you looked at your finger in front of your eyes, with one eye closed it looks as though it is in a different place than with the other eye or with both eyes open. Using both eyes your brain interprets the appropriate depth perception.
There are two main regions that surround the primary cortex that are usually referred to as areas V2 and V3 (the primary visual cortex is area V1). These surrounding areas are the visual association cortex. The visual association regions develop more complex visual perceptions by adding color and motion information. The information processed in these areas is then sent to regions of the temporal and parietal lobes. Visual processing has two separate streams of processing: one into the temporal lobe and one into the parietal lobe. These are the ventral and dorsal streams, respectively (Figure). The ventral stream identifies visual stimuli and their significance. Because the ventral stream uses temporal lobe structures, it begins to interact with the non-visual cortex and may be important in visual stimuli becoming part of memories. The dorsal stream locates objects in space and helps in guiding movements of the body in response to visual inputs. The dorsal stream enters the parietal lobe, where it interacts with somatosensory cortical areas that are important for our perception of the body and its movements. The dorsal stream can then influence frontal lobe activity where motor functions originate.
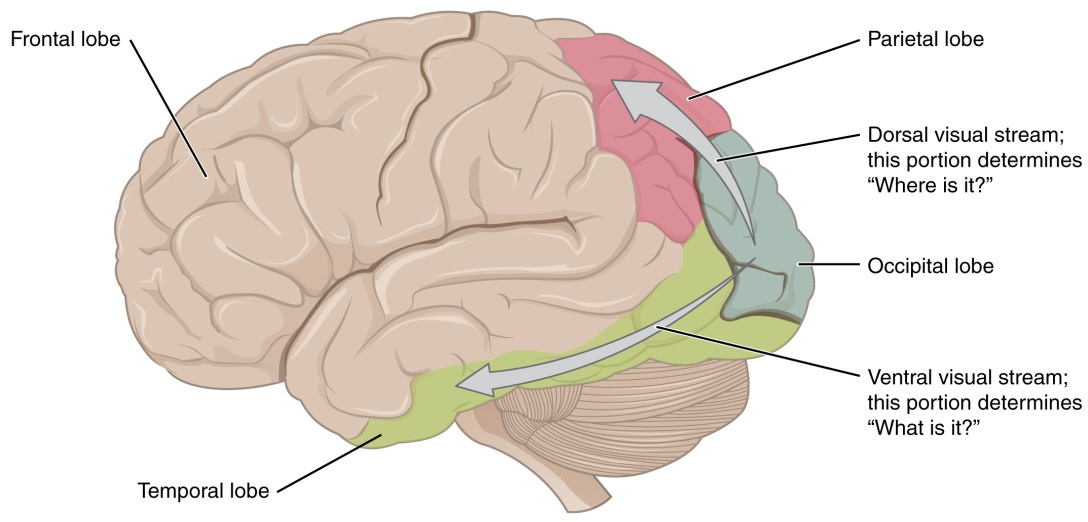
Figure 9: From the primary visual cortex in the occipital lobe, visual processing continues in two streams—one into the temporal lobe, which determines "What is it I am seeing?", and one into the parietal lobe, which determines "Where is it?"

Except where otherwise noted, this work by The Community College Consortium for Bioscience Credentials is licensed under a Creative Commons Attribution 4.0 International License.
Text from BioBook licensed under CC BY NC SA and Boundless Biology Open Textbook licensed under CC BY SA.
Other text from OpenStaxCollege licensed under CC BY 3.0. Modified by Alice Rudolph, M.A., Andrea Doub, M.S., Dr. Kim McMasters, D.C. and Amy Baugess, M.S. for c3bc.
Instructional Design by Courtney A. Harrington, Ph.D., Helen Dollyhite, M.A. and Caroline Smith, M.A. for c3bc.
Media by Brittany Clark, Jose DeCastro, Jordan Campbell and Antonio Davis for c3bc.
This product was funded by a grant awarded by the U.S. Department of Labor's Employment and Training Administration. The product was created by the grantee and does not necessarily reflect the official position of the U.S. Department of Labor. The Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership.