Anatomy of the Spinal Cord and Spinal Nerves
Anatomy & Physiology I
By the end of this section, the student will be able to:
The central nervous system (CNS) contains the brain and spinal cord, and the peripheral nervous system (PNS) is everything else. The spinal cord is the extension of nervous tissue in the vertebral column contained within the vertebral cavity. As the spinal cord continues to develop in the newborn, anatomical features mark its surface. For instance, the anterior midline is marked by the anterior median fissure, and the posterior midline is marked by the posterior median sulcus.
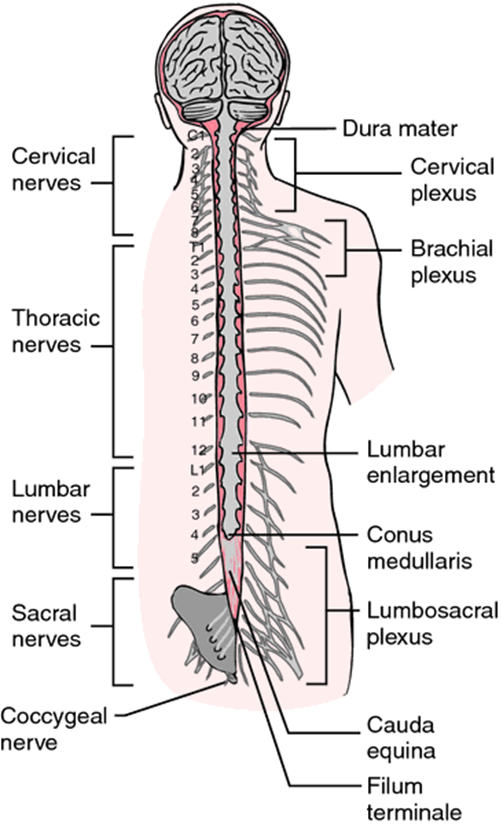
The length of the spinal cord is divided into regions that correspond to the regions of the vertebral column. The name of a spinal cord region corresponds to the level at which spinal nerves pass through the intervertebral foramina. Immediately inferior to the brain stem is the cervical region, followed by the thoracic, then the lumbar, and finally the sacral region. The spinal cord is not the full length of the vertebral column because the spinal cord does not grow significantly longer after the first or second year, but the skeleton continues to grow. The nerves that emerge from the lower spinal cord pass through the intervertebral formina at the respective levels. As the vertebral column grows, these nerves grow with it and result in a long bundle of nerves that resembles a horse's tail and is named the cauda equina. The sacral spinal cord is at the level of the upper lumbar vertebral bones. The spinal nerves extend from their various levels to the proper level of the vertebral column.
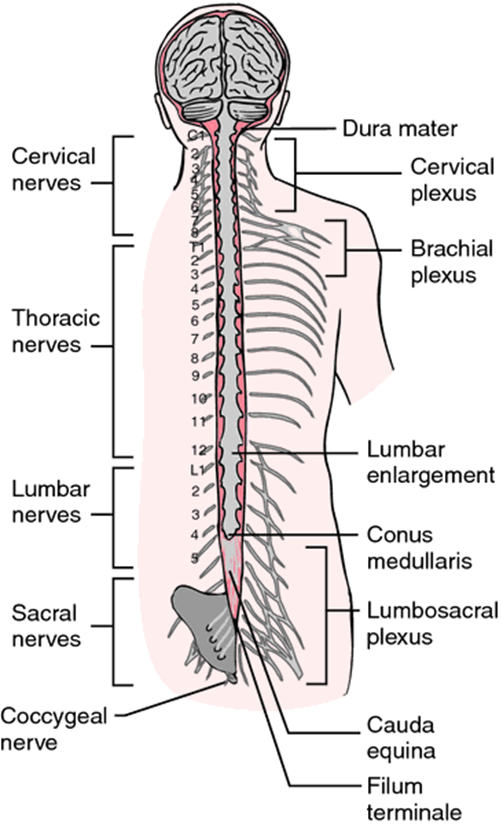
Figure 1. The spinal cord is not the full length of the vertebral column and it ends at the conus medullaris, usually around L1 or L2 on the vertebral column. The nerves that emerge from the lower spinal cord result in a long bundle of nerves that resembles a horse's tail and is named the cauda equina. The connective tissue anchor that extends from the conus medullaris down to the coccyx is the filum terminale, which helps to stabilize the cord in the subarachnoid space (along with denticulate ligaments that extend from the pia mater to the dura mater further anchoring the cord).
The end of the spinal cord containing cell bodies for motor neurons leaving the CNS is at the conus medullaris (about L1 to L2). This area is where the final nerves to and from the lower extremities enter or exit the spinal cord (remember that each spinal nerve contians both sensory and motor neurons communicating with the CNS). The next figure shows you the cauda equina of the spinal cord where the lumbar and sacral neurons extend from the end of the spinal cord and reach out (via intervertebral foramina) to the lower areas of the body.
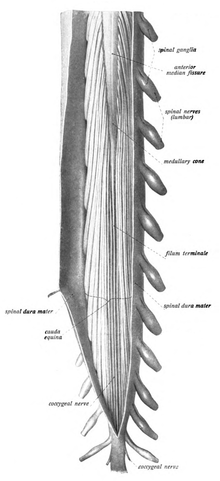
Figure 2. A dissection of the spinal cord showing the conus medullaris (the end of the spinal cord shaped like a cone in the middle of the nerves seen there), the cauda equina (looks like a horse's tail), and the filum terminale (the anchor to the spinal cord). By Dr. Johannes Sobotta - Sobotta's Textbook and Atlas of Human Anatomy 1908
The nerves connected to the spinal cord are the spinal nerves. All of the spinal nerves are combined sensory and motor axons that separate into two nerve roots. The sensory axons enter the spinal cord as the dorsal nerve root. The motor fibers, both somatic and autonomic, emerge as the ventral nerve root. The dorsal root ganglion found only on the dorsal root (hence its name) is made of the large conglomerated neuronal cell bodies packed into the ganglion.
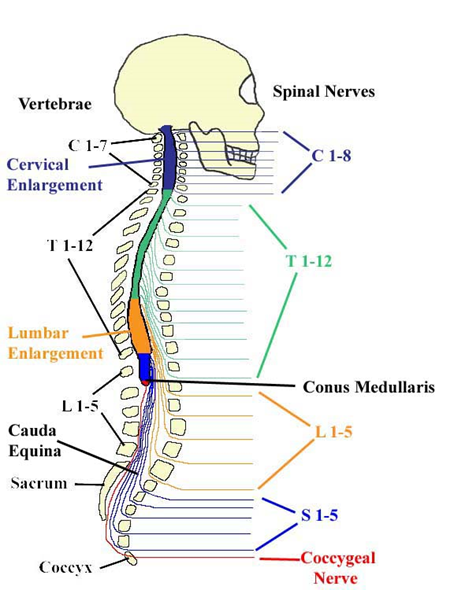
Figure 3. A skeleton view of the Spinal Cord, including where to find the 31 spinal nerves, the two spinal cord enlargements, and the location of the conus medullaris.
There are 31 spinal nerves, named for the level of the spinal cord at which each one emerges. There are eight pairs of cervical nerves designated C1 to C8, twelve thoracic nerves designated T1 to T12, five pairs of lumbar nerves designated L1 to L5, five pairs of sacral nerves designated S1 to S5, and one pair of coccygeal nerves. The nerves are numbered from the superior to inferior positions, and each emerges from the vertebral column through the intervertebral foramen at its level. The first nerve, C1, emerges between the first cervical vertebra and the occipital bone. The second nerve, C2, emerges between the first and second cervical vertebrae. The same occurs for C3 to C7, but C8 emerges between the seventh cervical vertebra and the first thoracic vertebra. For the thoracic and lumbar nerves, each one emerges between the vertebra that has the same designation and the next vertebra in the column. The sacral nerves emerge from the sacral foramina along the length of that unique vertebra.
Spinal nerves of the thoracic region, T2 through T11, are not part of the plexuses but rather emerge and give rise to the intercostal nerves found between the ribs, which articulate with the vertebrae surrounding the spinal nerve.
Spinal nerves extend outward from the vertebral column to innervate the periphery. The nerves in the periphery are not straight continuations of the spinal nerves, but rather the reorganization of the axons in those nerves to follow different courses. Axons from different spinal nerves will come together into a systemic nerve. This occurs at four places along the length of the vertebral column, each identified as a nerve plexus, whereas the other spinal nerves directly correspond to nerves at their respective levels. In this instance, the word plexus is used to describe networks of nerve fibers with no associated cell bodies.
There are four main nerve plexuses in the human body. The cervical plexus supplies nerves to the posterior head and neck, as well as the phrenic nerve to the diaphragm. The brachial plexus supplies five primary nerves to the arm - axillary, median, musculocutaneous, radial and ulnar nerves. The lumbar plexus supplies the femoral and other nerves to the anterior leg. The sacral plexus leads to the sciatic nerve and supplies nerves to the posterior leg. The location of the conus medularis lies about the area of L1 and L2, above the iliac crests.
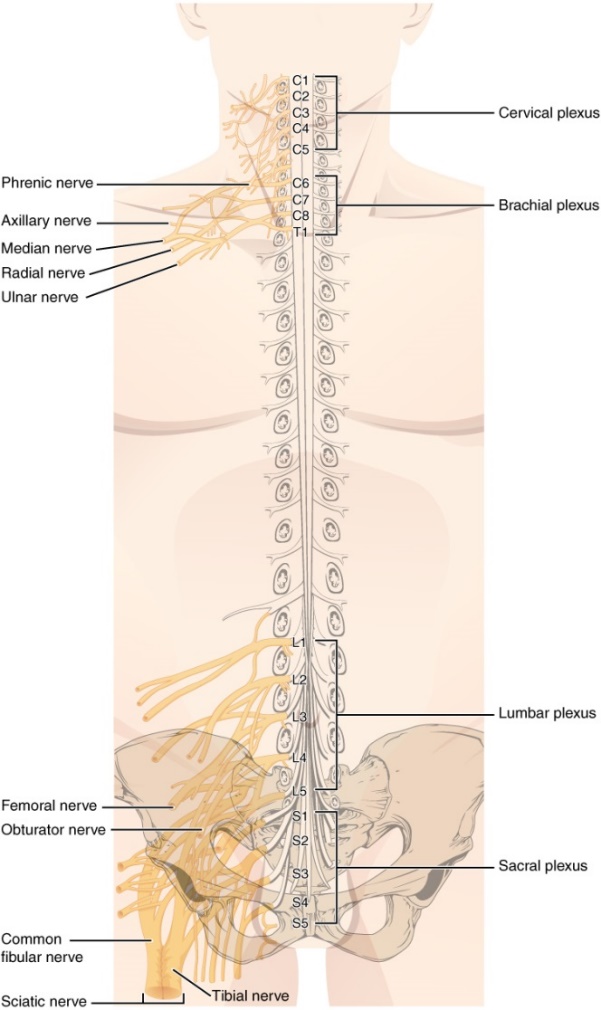
Figure 4 . There are four main nerve plexuses in the human body and 31 spinal nerves surrounded by the dura mater. The plexus networks are the cervical plexus, the brachial plexus, the lumbar plexus, and the sacral plexus (or the lumbosacral plexus). There are two enlargements, cervical enlargement and the lumbar enlargement, where a group of neuron cell bodies are located that supply the nerves to the large plexuses. Notice that the thoracic nerves do not have a plexus corresponding to them. Can you think of why?
{Response: There are ribs in the way so that the interconnections of a plexus network cannot be formed.}
Generally, spinal nerves contain afferent axons from sensory receptors in the periphery, such as from the skin, mixed with efferent axons travelling to the muscles or other effector organs. As the spinal nerve nears the spinal cord, it splits into dorsal and ventral roots. The dorsal root contains only the axons of sensory neurons, whereas the ventral roots contain only the axons of the motor neurons. Some of the branches will synapse with local neurons in the dorsal root ganglion, posterior (dorsal) horn, or even the anterior (ventral) horn, at the level of the spinal cord where they enter. Other branches will travel a short distance up or down the spine to interact with neurons at other levels of the spinal cord. A branch may also turn into the posterior (dorsal) column of the white matter to connect with the brain. For the sake of convenience, we will use the terms ventral and dorsal in reference to structures within the spinal cord that are part of these pathways. This will help to underscore the relationships between the different components. Typically, spinal nerve systems that connect to the brain are contralateral, in that the right side of the body is connected to the left side of the brain and the left side of the body to the right side of the brain.
Axons enter the posterior side through the dorsal (posterior) nerve root, which carries sensory information into the CNS. The axons emerging from the anterior side do so through the ventral (anterior) nerve root carrying motor information from the CNS . Note that it is common to see the terms dorsal (dorsal = "back") and ventral (ventral = "belly") used interchangeably with posterior and anterior, particularly in reference to nerves and the structures of the spinal cord. You should learn to be comfortable with both.
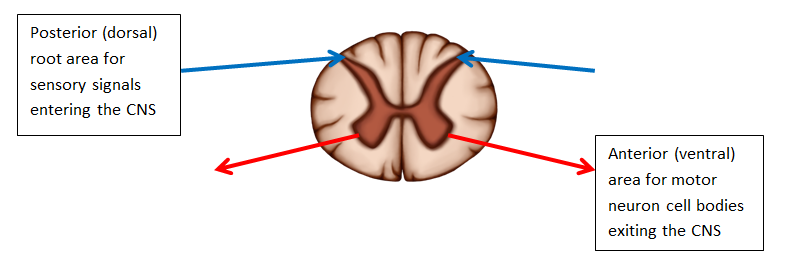
Figure 5. Spinal Cord Cross Section. The posterior/dorsal regions are responsible for receiving sensory functions and the anterior/ventral regions are associated with corresponding motor functions.
On the whole, the posterior regions are responsible for sensory functions and the anterior regions are associated with motor functions. This comes from the initial development of the spinal cord, which is divided into the basal plate and the alar plate. The basal plate is closest to the ventral midline of the neural tube, which will become the anterior face of the spinal cord and gives rise to motor neurons. The alar plate is on the dorsal side of the neural tube and gives rise to neurons that will receive sensory input from the periphery.
The somatic nervous system provides output strictly to skeletal muscles. The lower motor neurons, which are responsible for the contraction of these muscles, are found in the ventral horn of the spinal cord. These large, multipolar neurons have a corona of dendrites surrounding the cell body and an axon that extends out of the ventral horn. This axon travels through the ventral nerve root to join the emerging spinal nerve. The axon is relatively long because it needs to reach muscles in the periphery of the body. The diameters of cell bodies may be on the order of hundreds of micrometers to support the long axon; some axons are a meter in length, such as the lumbar motor neurons that innervate muscles in the first digits of the feet.
The axons will also branch to innervate multiple muscle fibers. Together, the motor neuron and all the muscle fibers that it controls make up a motor unit. Motor units vary in size. Some may contain up to 1000 muscle fibers, such as in the quadriceps, or they may only have 10 fibers, such as in an extraocular muscle. The number of muscle fibers that are part of a motor unit corresponds to the precision of control of that muscle. Also, muscles that have finer motor control have more motor units connecting to them, and this requires a larger topographical field in the primary motor cortex.
Motor neuron axons connect to muscle fibers at a neuromuscular junction. This is a specialized synaptic structure at which multiple axon terminals synapse with the muscle fiber sarcolemma. The synaptic end bulbs of the motor neurons secrete acetylcholine, which binds to receptors on the sarcolemma. The binding of acetylcholine opens ligand-gated ion channels, increasing the movement of cations across the sarcolemma. This depolarizes the sarcolemma, initiating muscle contraction. Whereas other synapses result in graded potentials that must reach a threshold in the postsynaptic target, activity at the neuromuscular junction reliably leads to muscle fiber contraction with every nerve impulse received from a motor neuron. However, the strength of contraction and the number of fibers that contract can be affected by the frequency of the motor neuron impulses.
In cross-section, the gray matter of the spinal cord has the appearance of an ink-blot test, with the spread of the gray matter on one side replicated on the other—a shape reminiscent of a swollen capital "H." As shown in Figure 4, the gray matter is subdivided into regions that are referred to as horns. The posterior horn is responsible for sensory processing. The anterior horn sends out motor signals to the skeletal muscles. The lateral horn, which is only found in the thoracic, upper lumbar, and sacral regions, is the central component of the sympathetic division of the autonomic nervous system.
Some of the largest neurons of the spinal cord are the multipolar motor neurons in the anterior horn. The fibers that cause contraction of skeletal muscles are the axons of these neurons. The motor neuron that causes contraction of the big toe, for example, is located in the sacral spinal cord. The axon that has to reach all the way to the belly of that muscle may be a meter in length. The neuronal cell body maintaining that long axonal fiber is quite large, possibly several hundred micrometers in diameter, and makes it one of the largest cells in the body.
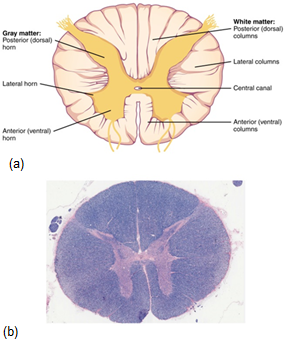
Figure 6. (a) The cross-section of a thoracic spinal cord segment shows the posterior, anterior, and lateral horns of gray matter, which make the shape of an "H" in the middle of the spinal cord. Also shown are the posterior, anterior, and lateral columns of white matter, which surround this letter "H". In the center of the gray matter ("H") is found the small Central Canal, which holds cerebrospinal fluid. LM × 40. (b) shows an actual micrograph provided by the Regents of University of Michigan Medical School © 2012
Just as the gray matter is separated into horns, the white matter of the spinal cord is separated into columns. Ascending tracts of nervous system fibers in these columns carry sensory information up to the brain, whereas descending tracts carry motor commands from the brain. Looking at the spinal cord longitudinally, the column-like tracts extend along its length as continuous bands of white matter. Between the two posterior horns of gray matter are the posterior columns of white matter . Between the two anterior horns, and bounded by the axons of motor neurons emerging from that gray matter area, are the anterior columns. The white matter on either side of the spinal cord, between the posterior horn and the axons of the anterior horn neurons, are the lateral columns. The posterior columns are composed of axons of ascending tracts. The anterior and lateral columns are composed of many different groups of axons of both ascending and descending tracts — the latter carrying motor commands down from the brain to the spinal cord to control output to the periphery.
Also, remember the anterior midline is marked by the anterior median fissure, and the posterior midline is marked by the posterior median sulcus. Can you find these on the figure below?
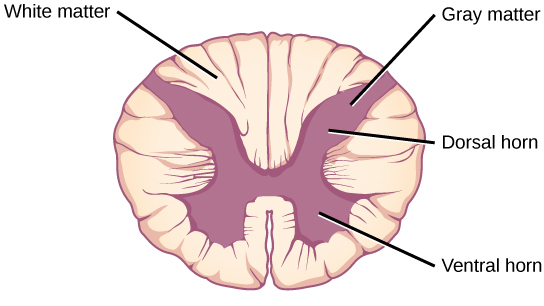
Figure 7. A cross-section of the spinal cord shows gray matter (containing cell bodies and unmyelinated interneurons) and white matter (containing myelinated axons).
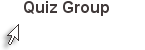
Notice in the spinal cord that the amount of gray and white matter fluctuates as the nerves "jump on" or "jump off." Where in the cord is there more white matter? Remember what is held in the white matter? So why is there more white matter as you ascend the spinal cord? See the figure below.
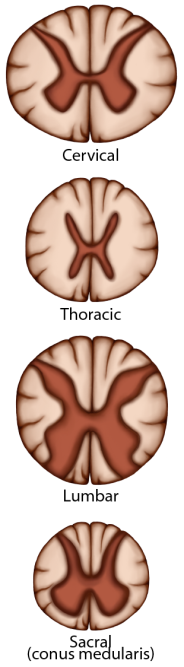
Figure 8. From superior to inferior, the spinal cord becomes smaller. There is less and less white matter as it descends because there are fewer afferent tracts going up (they haven't "jumped on" yet), and there are fewer efferent tracts going down (they've "jumped off" already.) The sacral nerves are actually in the area close to the lumbar enlargement and the conus medullaris, since they will leave at the end of the spinal cord.
A sensory pathway that carries peripheral sensations to the brain is referred to as an ascending pathway, or ascending tract. The various sensory modalities each follow specific pathways through the CNS. Tactile and other somatosensory stimuli activate receptors in the skin, muscles, tendons, and joints throughout the entire body. However, the somatosensory pathways are divided into two separate systems on the basis of the location of the receptor neurons. Somatosensory stimuli from below the neck pass along the sensory pathways of the spinal cord, whereas somatosensory stimuli from the head and neck travel through the cranial nerves—specifically, the trigeminal system.
The dorsal column system (sometimes referred to as the dorsal (or posterior) column-medial lemniscus) and the spinothalamic tract are two major pathways that bring sensory information to the brain (Figure). The sensory pathways in each of these systems are composed of three successive neurons.
The dorsal column system begins with the axon of a dorsal root ganglion neuron entering the dorsal root and joining the dorsal column white matter in the spinal cord. As axons of this pathway enter the dorsal column, they take on a positional arrangement so that axons from lower levels of the body position themselves medially, whereas axons from upper levels of the body position themselves laterally. The dorsal column is separated into two component tracts, the fasciculus gracilis that contains axons from the legs and lower body, and the fasciculus cuneatus that contains axons from the upper body and arms.
The axons in the dorsal column terminate in the nuclei of the medulla, where each synapses with the second neuron in their respective pathway. The nucleus gracilis is the target of fibers in the fasciculus gracilis, whereas the nucleus cuneatus is the target of fibers in the fasciculus cuneatus. The second neuron in the system projects from one of the two nuclei and then decussates, or crosses the midline of the medulla. These axons then continue to ascend the brain stem as a bundle called the medial lemniscus. These axons terminate in the thalamus, where each synapses with the third neuron in their respective pathway. The third neuron in the system projects its axons to the postcentral gyrus of the cerebral cortex, where somatosensory stimuli are initially processed and the conscious perception of the stimulus occurs.
The spinothalamic tract also begins with neurons in a dorsal root ganglion. These neurons extend their axons to the dorsal horn, where they synapse with the second neuron in their respective pathway. The name "spinothalamic" comes from this second neuron, which has its cell body in the spinal cord gray matter and connects to the thalamus. Axons from these second neurons then decussate within the spinal cord and ascend to the brain and enter the thalamus, where each synapses with the third neuron in its respective pathway. The neurons in the thalamus then project their axons to the spinothalamic tract, which synapses in the postcentral gyrus of the cerebral cortex.
These two systems are similar in that they both begin with dorsal root ganglion cells, as with most general sensory information. The dorsal column system is primarily responsible for touch sensations and proprioception, whereas the spinothalamic tract pathway is primarily responsible for pain and temperature sensations. Another similarity is that the second neurons in both of these pathways are contralateral, because they project across the midline to the other side of the brain or spinal cord. In the dorsal column system, this decussation takes place in the brain stem; in the spinothalamic pathway, it takes place in the spinal cord at the same spinal cord level at which the information entered. The third neurons in the two pathways are essentially the same. In both, the second neuron synapses in the thalamus, and the thalamic neuron projects to the somatosensory cortex.
The left panel shows the dorsal column system and its connection to the brain. The right column shows the spinothalamic tract and its connection to the brain.
The dorsal column system and spinothalamic tract are the major ascending pathways that connect the periphery with the brain.
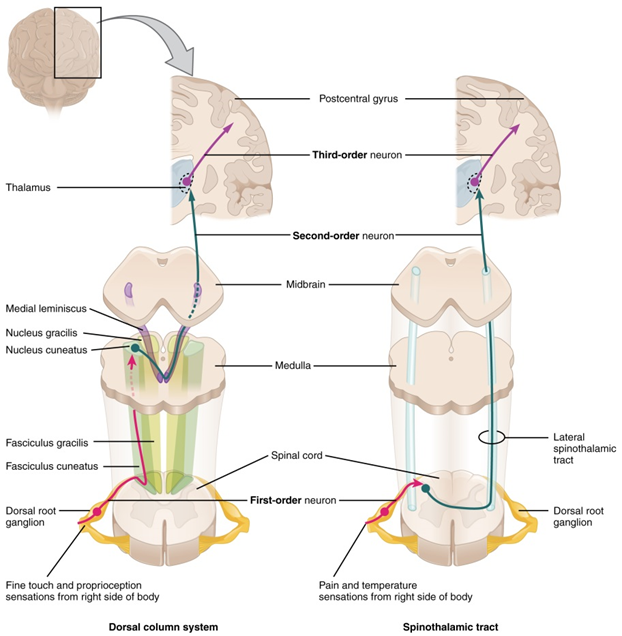
Figure 9. The dorsal column system and spinothalamic tract (both seen here with blue arrows) are the major ascending pathways that connect the periphery with the brain.
The lateral corticospinal tract is composed of the fibers that cross the midline at the pyramidal decussation (see Figure). The axons cross over from the anterior position of the pyramids in the medulla to the lateral column of the spinal cord. These axons are responsible for controlling appendicular muscles.
This influence over the appendicular muscles means that the lateral corticospinal tract is responsible for moving the muscles of the arms and legs. The ventral horn in both the lower cervical spinal cord and the lumbar spinal cord both have wider ventral horns, representing the greater number of muscles controlled by these motor neurons. The cervical enlargement is particularly large because there is greater control over the fine musculature of the upper limbs, particularly of the fingers. The lumbar enlargement is not as significant in appearance because there is less fine motor control of the lower limbs.
The anterior corticospinal tract is responsible for controlling the muscles of the body trunk (see Figure). These axons do not decussate in the medulla. Instead, they remain in an anterior position as they descend the brain stem and enter the spinal cord. These axons then travel to the spinal cord level at which they synapse with a lower motor neuron. Upon reaching the appropriate level, the axons decussate, entering the ventral horn on the opposite side of the spinal cord from which they entered. In the ventral horn, these axons synapse with their corresponding lower motor neurons. The lower motor neurons are located in the medial regions of the ventral horn, because they control the axial muscles of the trunk.
Because movements of the body trunk involve both sides of the body, the anterior corticospinal tract is not entirely contralateral. Some collateral branches of the tract will project into the ipsilateral ventral horn to control synergistic muscles on that side of the body, or to inhibit antagonistic muscles through interneurons within the ventral horn. Through the influence of both sides of the body, the anterior corticospinal tract can coordinate postural muscles in broad movements of the body. These coordinating axons in the anterior corticospinal tract are often considered bilateral, as they are both ipsilateral and contralateral.
Figure 10. The major descending tract that controls skeletal muscle movements is the corticospinal tract. It is composed of two neurons, the upper motor neuron (yellow arrows) and the lower motor neuron (green arrow). The upper motor neuron has its cell body in the primary motor cortex of the frontal lobe, crosses over (or decussates) in the pyramids of the medulla, and synapses on the lower motor neuron, which is in the ventral horn of the spinal cord and projects to the skeletal muscle in the periphery.
Specific regions of the CNS coordinate different somatic processes using sensory inputs and motor outputs of peripheral nerves. A simple case is a reflex caused by a synapse between a dorsal sensory neuron axon and a motor neuron in the ventral horn. A simple reflex arc includes the sensory receptor, the sensory (afferent) neuron, an interneuron (except in monosynatpic arcs), the motor (efferent) neuron, and the effector (muscle or gland). More complex arrangements are possible to integrate peripheral sensory information with higher processes. The important regions of the CNS that play a role in somatic processes can be separated into the spinal cord brain stem, diencephalon, cerebral cortex, and subcortical structures.
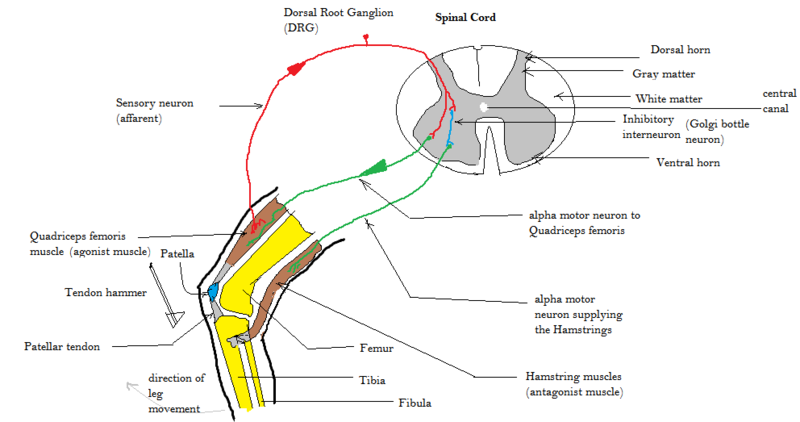
Figure 11. This figure shows a simple reflex of the spinal cord - the patellar reflex. The red arrow is the sensory neuron, which sends a signal to the gray matter of the spinal cord, when the leg muscle is stretched by the hammer hitting the patellar tendon. The green arrows show the two motor signals leaving the ventral horn to signal the opposing muscles. The quadriceps muscle will contract and the hamstring muscle will be inhibited and remain relaxed, thus extending the leg.
Several diseases can result from the demyelination of axons. The causes of these diseases are not the same; some have genetic causes, some are caused by pathogens, and others are the result of autoimmune disorders. Though the causes are varied, the results are largely similar. The myelin insulation of axons is compromised, making electrical signaling slower.
The symptoms of MS include both somatic and autonomic deficits. Control of the musculature is compromised, as is control of organs such as the bladder.
Parkinson's disease is neurodegenerative, meaning that neurons die that cannot be replaced, so there is no cure for the disorder. Treatments for Parkinson's disease are aimed at increasing dopamine levels in the striatum. Currently, the most common way of doing that is by providing the amino acid L-DOPA, which is a precursor to the neurotransmitter dopamine and can cross the blood-brain barrier. With levels of the precursor elevated, the remaining cells of the substantia nigra pars compacta can make more neurotransmitter and have a greater effect. Unfortunately, the patient will become less responsive to L-DOPA treatment as time progresses, and it can cause increased dopamine levels elsewhere in the brain, which are associated with psychosis or schizophrenia.

Except where otherwise noted, this work by The Community College Consortium for Bioscience Credentials is licensed under a Creative Commons Attribution 4.0 International License.
Text from BioBook licensed under CC BY NC SA and Boundless Biology Open Textbook licensed under CC BY SA.
Other text from OpenStaxCollege licensed under CC BY 3.0. Modified by Alice Rudolph, M.A., Andrea Doub, M.S. and Dr. Gustavo Solis, M.D. for c3bc.
Instructional Design by Courtney A. Harrington, Ph.D., Helen Dollyhite, M.A. and Caroline Smith, M.A. for c3bc.
Media by Brittany Clark, Jose DeCastro, Jordan Campbell and Antonio Davis for c3bc.
This product was funded by a grant awarded by the U.S. Department of Labor's Employment and Training Administration. The product was created by the grantee and does not necessarily reflect the official position of the U.S. Department of Labor. The Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership.