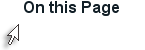
Epidermal Layers
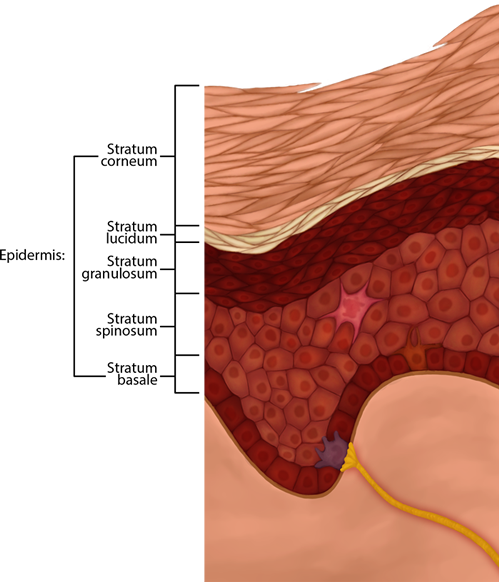
Figure 3. Micrographic Representation of the Epidermal Skin Layers Described Below
The Five Layers of the Epidermis (from superficial to deep) Include:
- Stratum Corneum: about 20 layers of squamous-shaped dead cells (dead due to all the keratin) providing a layer of water resistance (not water-proof, though); thicker Corneum (with more layers) in the palms and heels and thinner elsewhere on the body; these dead keratinocytes are regularly sloughed away, being replaced by cells from the deeper layers. This dry, dead layer helps prevent the penetration of microbes and the dehydration of underlying tissues, and provides a mechanical protection against abrasion for the more delicate, underlying layers, so it is your first line of defense.
- Stratum Lucidum: this layer is more translucent or clear (due to special proteins that are clear) and are dead cells providing an extra water barrier. It is only seen in thick skin of the fingertips, palms and soles of the feet, though.
- Stratum Granulosum: cells here (three to five layers deep) become flatter, their cell membranes thicken, and they generate large amounts of the protein keratin, which is fibrous; as the cells die, they leave behind the keratin, etc. that form the stratum lucidum, the stratum corneum, and the layers of our hair and nails.
- Stratum Spinosum: these cells have bundles of protein filaments (beginning to make keratin) and they look prickly/spiny under the microscope.
- Stratum Basale: (pronounced BAY-zal-ee) The most deep layer, next to the basement membrane; stem cells here divide by mitosis, work their way up, to replace more superficial cells being lost at surface. Of the two other cells in this layer, one is the Merkel's disc, which functions as a receptor and perceives sensations of touch. These cells are found mostly on the surfaces of the hands and feet. Melanocytes dwell here as well and produce the pigment melanin, that permeates into developing keratinocytes, which protects lower layers from UV light. Albinos' melanocytes do not make melanin, but we all have the same amount of melanocytes. Malignant melanoma is a cancer of melanocytes. Basal cell carcinoma originates from this layer, too. These specialized cells are labeled below in Figure 4.
Figure 4. Specialized Epidermal Cell include Langerhans Cells for immune function, melanocytes, Merkel cells, and tactile discs.
![]()
![]()
Video 1. View the Epidermis video on YouTube (opens in new window)
Think About This: If the number of melanocytes is the same in people of all ethnic backgrounds, what causes their skin color to differ?
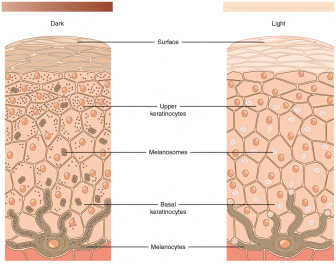
Figure 5. Melanocytes are found in the Stratum Basale. Cytoplasmic extensions reach into the Stratum Spinosum, though, filled with protein (pigment) molecules as long as the person's DNA is programmed to produce them. The Light skin on the left has the melanocyte, but it is not producing much melanin, or pigment proteins, whereas the Dark skin on the right is forming more of the protein melanin. The Dark skin has melanosome organelles storing the pigments throughout the keratinocytes making the skin appear darker.
CC BY: OpenStax
Acronyms for the layers from superficial to deep, which help us remember the beginning letter(s) of the names of each stratum, include: Can Lucy Give Some Blood? or Corny Lucy's Grandma Spins Baseballs.
The first thing a clinician sees is the skin, and so the examination of the skin should be part of any thorough physical examination. Most skin disorders are relatively benign, but a few, including melanomas, can be fatal if untreated.